Camels and sharks have small, sneaky antibodies that can help fight human diseases
Sharks #Sharks

This article was originally featured in Knowable Magazine.
Every four months, pathologist Aaron LeBeau scoops into a net one of the five nurse sharks he keeps in his University of Wisconsin lab. Then he carefully administers a shot to the animal, much like a pediatrician giving a kid a vaccine. The shot will immunize the shark against a human cancer, perhaps, or an infectious disease, such as Covid-19. A couple of weeks later, after the animal’s immune system has had time to react, LeBeau collects a small vial of shark blood.
Halfway across the country, immunologist Hidde Ploegh goes through the same steps, but with alpacas that live on a farm in western Massachusetts. The scientists are after the same thing: tiny antibodies, made only by certain animals, that may have big implications for human health.
Most antibodies — those molecules that course through our blood and tissues patrolling for pathogens — are fairly hefty as proteins go. But the antibodies made by camels and sharks and their close relatives are simpler and smaller. Since their discovery in the late 1980s, researchers have learned that these antibodies pack a big punch: They can latch onto hidden parts of molecules and can penetrate tissues more deeply, enhancing their potential as therapies.
“They can get into little nooks and crannies of different proteins that human antibodies cannot access,” LeBeau says.
In the last decades, investigations of these diminutive antibodies have surged. Not only can they sneak into small places, they are also easy to work with — sturdier than their ordinary counterparts — and relatively cheap to make in large quantities. All these features make the antibodies promising treatments for a host of diseases, whether clotting disorders or Covid-19. Researchers are also exploring their use for diagnosing conditions such as cancer, and they’re becoming a key tool in other kinds of research, like mapping cells’ insides.
The full promise of these antibodies may still take years to realize, but researchers are very excited about their possibilities. “I think they have potential to save the world,” LeBeau says.
Luck of the blood draw
A group of biology students were the first to discover these unusual antibodies — quite by chance — back in 1989. The students of Free University in Brussels needed some blood for an exam in which they were tasked with separating an antibody into its two main parts: two heavy protein chains, which form a Y shape, and two light protein chains, which flank the prongs at the top of the Y.
Human blood seemed too risky to work with, given concerns at the time about potential HIV exposure, and the students didn’t want to kill a mouse. But the students’ professor, the late Raymond Hamers, happened to be studying sleeping sickness in large animals. He gave the students some blood from a camel, says immunologist Serge Muyldermans, who was then a post-doctoral researcher at the university.
Strangely, the students found only heavy chain proteins in the blood even though antibodies were supposed to also have light chains. As Muyldermans tells it, everyone thought that the camel antibodies had degraded — or that the students had done something wrong — so Hamers went to the Antwerp Zoo to collect fresh camel blood. But the students had not screwed up: Camels make antibodies with only heavy protein chains.
The potential applications of camelids’ small antibodies dawned on Hamers during those early years, says Muyldermans, who details their myriad uses in the 2021 Annual Review of Animal Biosciences. Like antibodies from people or mice, the camelid antibodies could be further pared down into even smaller, yet still effective, fragments — just the tips of the Y. These fragments, called variable domains, are the business end of any antibody — they act as the antibody’s “sensor” and can stick to parts of pathogens or toxins, whatever substance is recognized as foreign and a possible threat.
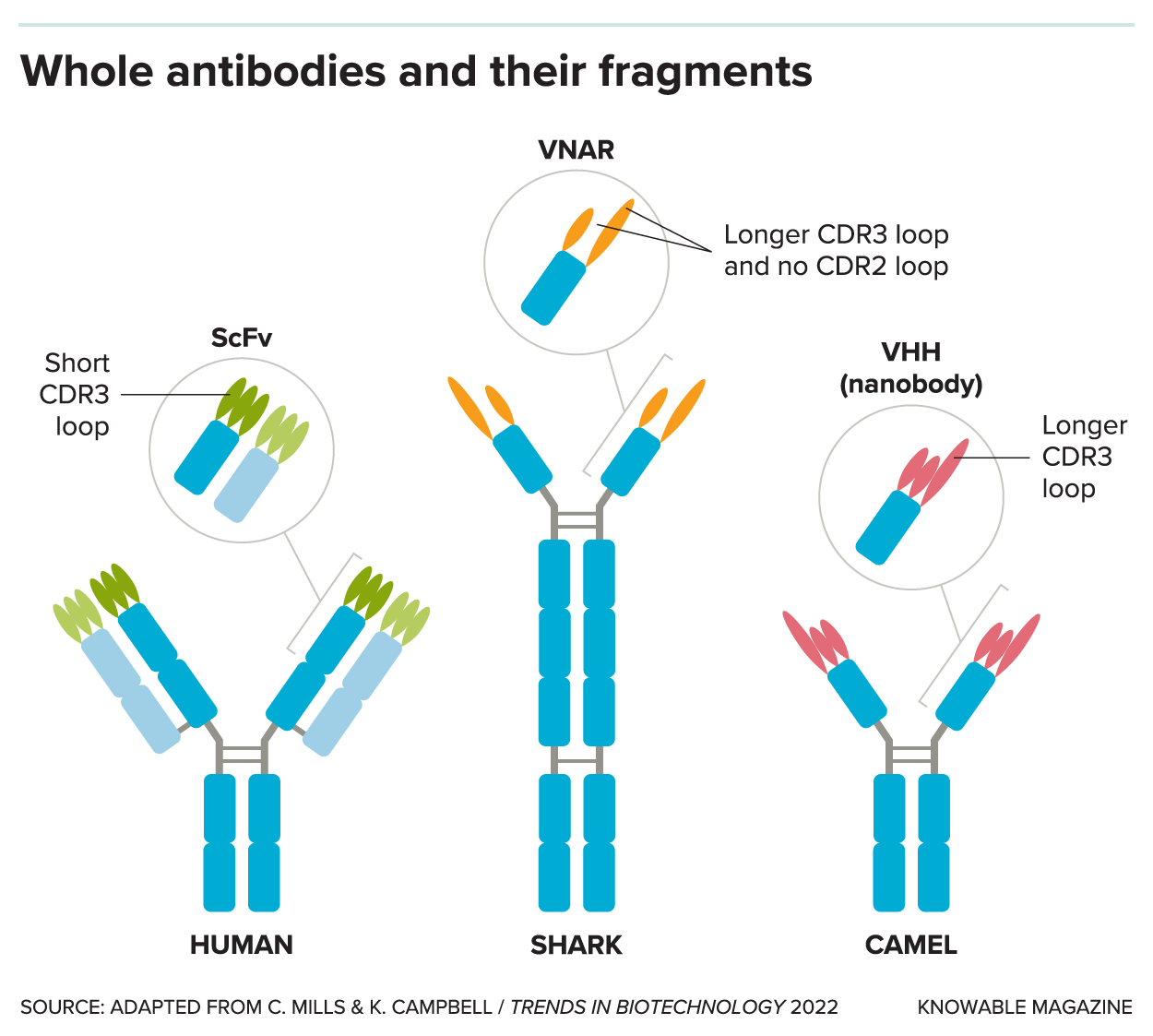 Full-size antibodies, like those of humans (left), typically have heavy protein chains (dark blue) and light protein chains (light blue). In addition to these standard antibodies, sharks and camels and their relatives make antibodies with only heavy chains (middle and right). The fragments at the antibody tips (shown in circles), called variable domains, stick to parts of pathogens or toxins, whatever substance is recognized as foreign to the body. The variable domains of sharks (VNARs, middle) and camels (VHHs, or nanobodies, right) have an extra-long fingerlike extension, called the CDR3 loop, that can reach into nooks and crannies inaccessible to a standard antibody fragment (ScFv, left).
Full-size antibodies, like those of humans (left), typically have heavy protein chains (dark blue) and light protein chains (light blue). In addition to these standard antibodies, sharks and camels and their relatives make antibodies with only heavy chains (middle and right). The fragments at the antibody tips (shown in circles), called variable domains, stick to parts of pathogens or toxins, whatever substance is recognized as foreign to the body. The variable domains of sharks (VNARs, middle) and camels (VHHs, or nanobodies, right) have an extra-long fingerlike extension, called the CDR3 loop, that can reach into nooks and crannies inaccessible to a standard antibody fragment (ScFv, left).
In standard antibodies (which camels also make), the variable domains come in pairs, one from the heavy chain and one from the light chain. But the variable domains of the camelid’s heavy-chain-only antibodies are singletons. The researchers realized these solitary fragments might be able to grab onto parts of foreign molecules that conventional antibodies were too bulky to reach.
In 1993, the team published the discovery in Nature. The next year, Hamers patented the production of these camelid antibody fragments (they are also known as VHH antibodies or “nanobodies,” a trademarked term). A few years later, a different group of researchers reported that sharks also make antibodies with only heavy chains and these have an even smaller tip (these shark end fragments are called variable new antigen receptors, or VNARs).
When the primary patent expired in 2013, research investigating the antibodies really surged, says Ploegh, an immunologist at Boston Children’s Hospital. “That’s sort of when the dam broke and a lot of folks got in on the game.”
Scientists have since learned a lot about the advantages of these mini antibodies. Some is practical: Unlike full-size antibodies, the fragments are stable at room temperature so there’s no need to keep them in a freezer or ship them cold. The mini antibodies of sharks can even be boiled with no effect on their function, LeBeau says. And while full-size antibodies require mammalian cells to be grown in a flask, which can be complicated and expensive to maintain, the fragments can be manufactured in large quantities using bacteria, saving time and money.
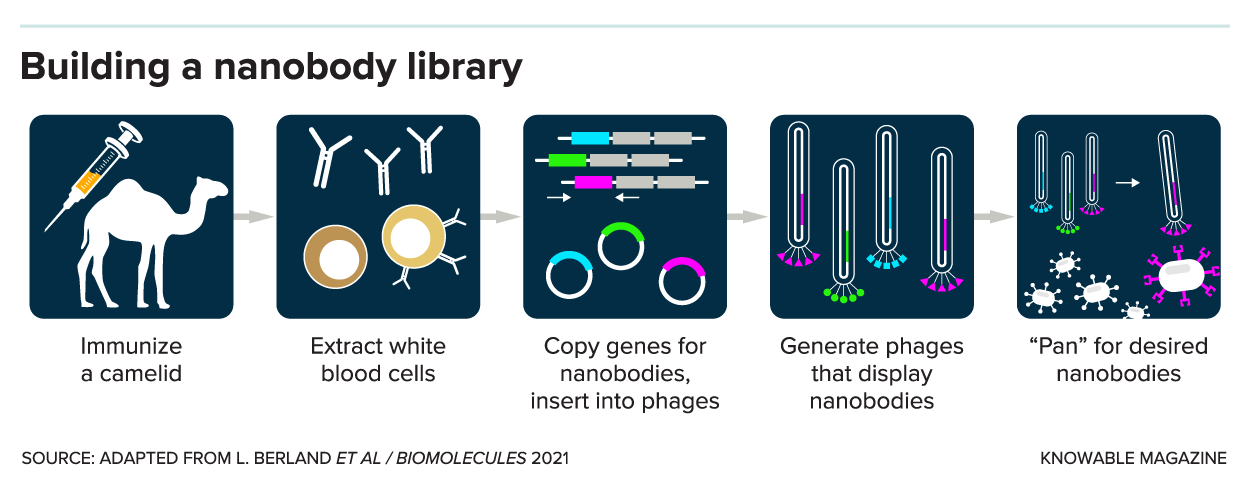 Scientists are investigating nanobodies and their diminutive brethren for all sorts of purposes. This research may begin by building a nanobody library: To identify antibody fragments that work against a specific target, like SARS-CoV-2 or a cancer protein, researchers often start by immunizing a camel or shark with their target of interest. A few weeks later, they take blood from the animal to get white blood cells. From those white blood cells, they make copies of the antibodies’ genes to insert into viruses called bacteriophages that display the nanobodies on their surface. Researchers can then sort through those nanobodies, like panning for gold to find the ones that attach to their protein of interest.
Scientists are investigating nanobodies and their diminutive brethren for all sorts of purposes. This research may begin by building a nanobody library: To identify antibody fragments that work against a specific target, like SARS-CoV-2 or a cancer protein, researchers often start by immunizing a camel or shark with their target of interest. A few weeks later, they take blood from the animal to get white blood cells. From those white blood cells, they make copies of the antibodies’ genes to insert into viruses called bacteriophages that display the nanobodies on their surface. Researchers can then sort through those nanobodies, like panning for gold to find the ones that attach to their protein of interest.
These mini antibodies also tend to self-assemble properly, keeping their correct shapes, making them a promising alternative to full-size antibodies, which have more pieces and thus can misfold. Such misfolding may expose parts that are more likely to be recognized by the immune system as foreign molecules, which can provoke a negative immune response in the body, with potentially serious consequences for patient health.
But the standout trait of the mini antibodies is their versatility. All antibodies, whether from human or shark, have variable domains at their tips, but those of sharks and camels have unique traits. They have an especially long, slender finger called a CDR3 loop that can poke into places that human antibodies can’t access. They appear to easily adopt different shapes — LeBeau describes that feature as “molecular yoga.” This means mini antibodies can get into tight spots, whether into tissues of the body or on minuscule parts of individual molecules.
Anti-cancer antibodies
Research into these unusual mini antibodies is now starting to bear fruit. In 2019, the first mini antibody medical treatment to be approved by the US Food and Drug Administration, called Cablivi, came on the market. It treats a rare blood disorder that leads to clots in small blood vessels. The treatment uses nanobodies to bind to a protein in platelets, which stops them from sticking together.
Mini antibodies could become a valuable tool for cancer treatment. Full-size antibodies are already used in immunotherapies to treat certain cancers; in some cases, the antibody tags cancer cells so that the body’s own immune system cells can then recognize and kill the rogue cells; in others, it might bring immune cells closer to the cancer cells so the body can better fight the cancer. The mini antibodies can do the same tasks, but can also be used in other ways, such as targeting proteins to reduce tumor growth or blocking blood vessels from feeding a tumor. And the smaller antibodies also may be less likely to trigger a negative immune response than full-size immunotherapy antibodies, which may lead to dramatic treatment improvements, Ploegh says.
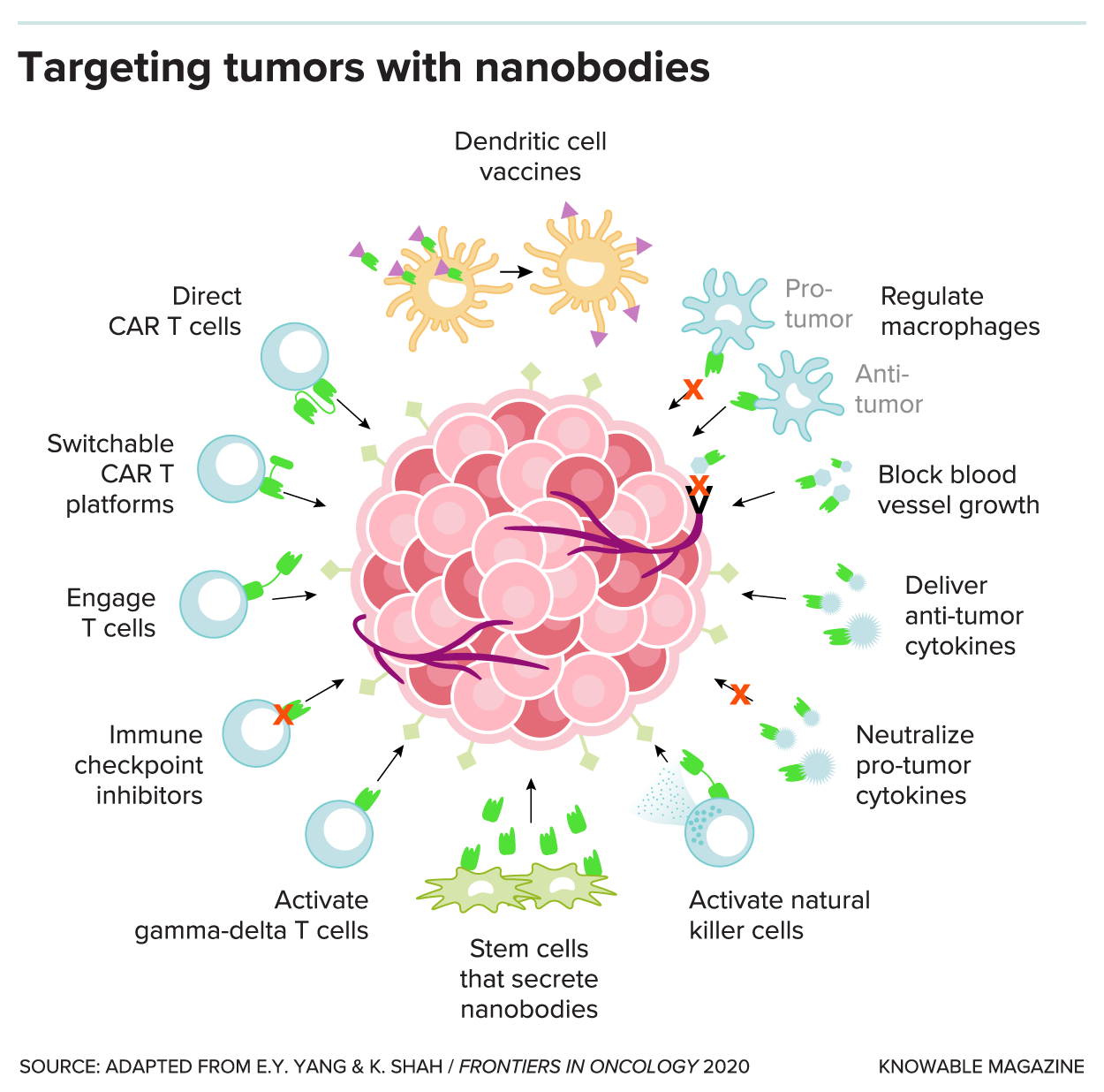 Full-sized antibodies are already used for cancer immunotherapy, harnessing the body’s various immune-system cells to help kill cancer cells. For example, T cells can be removed from the body and engineered to make a chimeric antigen receptor (CAR) that includes a human antibody fragment capable of recognizing certain kinds of cancer. Nanobodies can be used in the same tumor-attacking ways, such as targeting proteins to reduce tumor growth or blocking blood vessels from feeding a tumor.
Full-sized antibodies are already used for cancer immunotherapy, harnessing the body’s various immune-system cells to help kill cancer cells. For example, T cells can be removed from the body and engineered to make a chimeric antigen receptor (CAR) that includes a human antibody fragment capable of recognizing certain kinds of cancer. Nanobodies can be used in the same tumor-attacking ways, such as targeting proteins to reduce tumor growth or blocking blood vessels from feeding a tumor.
LeBeau, for his part, is focused on developing mini antibodies targeted for prostate and lung cancer. The sharks in his lab, each named for James Bond bad guys — Goldfinger, Hugo Drax, Mr. Stamper, Oddjob and Nick Nack — keep him supplied with antibodies that he uses in lab experiments. His lab recently identified a shark antibody fragment that is specific for a highly aggressive, and currently untreatable, form of lung cancer. He’s hopeful that this new mini antibody could help combat the cancer, and has studies in progress to test it.
The mini antibodies are also helping physicians detect cancers more readily, pinpointing diseased cells with more precision. By attaching radioactive tracer molecules to specific antibodies that seek out cancer cells, physicians can locate cancerous cells on a PET scan, potentially with greater resolution than with standard antibodies because they can penetrate deeper into tissues. One such nanobody-based tracer detected several tumors in mice with higher specificity than conventional imaging, a team reported in PNAS in 2019.
Vanquishing viruses
Scientists are also harnessing mini antibodies to fight infectious diseases, including Covid-19. Wai-Hong Tham, an infectious disease researcher at the University of Melbourne and the Walter and Eliza Hall Institute of Medical Research, has been working to generate nanobodies that grab onto part of the spike protein of SARS-CoV-2, to prevent the virus from entering cells in the body.
In a preliminary study, published in PNAS in 2021, Tham and her colleagues identified several nanobodies from alpacas that interfered with the spike proteins’ ability to latch onto the molecular doorknob it uses to get into cells; cocktails of the nanobodies also reduced the amount of virus in experiments with mice. Ideally, Tham says, they could find a nanobody that universally blocks Covid-19 regardless of the coronavirus variant. Other nanobody cocktails also appear promising: Four nanobodies, mixed and matched in various combinations, disabled the spike protein in experiments in cells, a separate team reported in 2021 in Science.
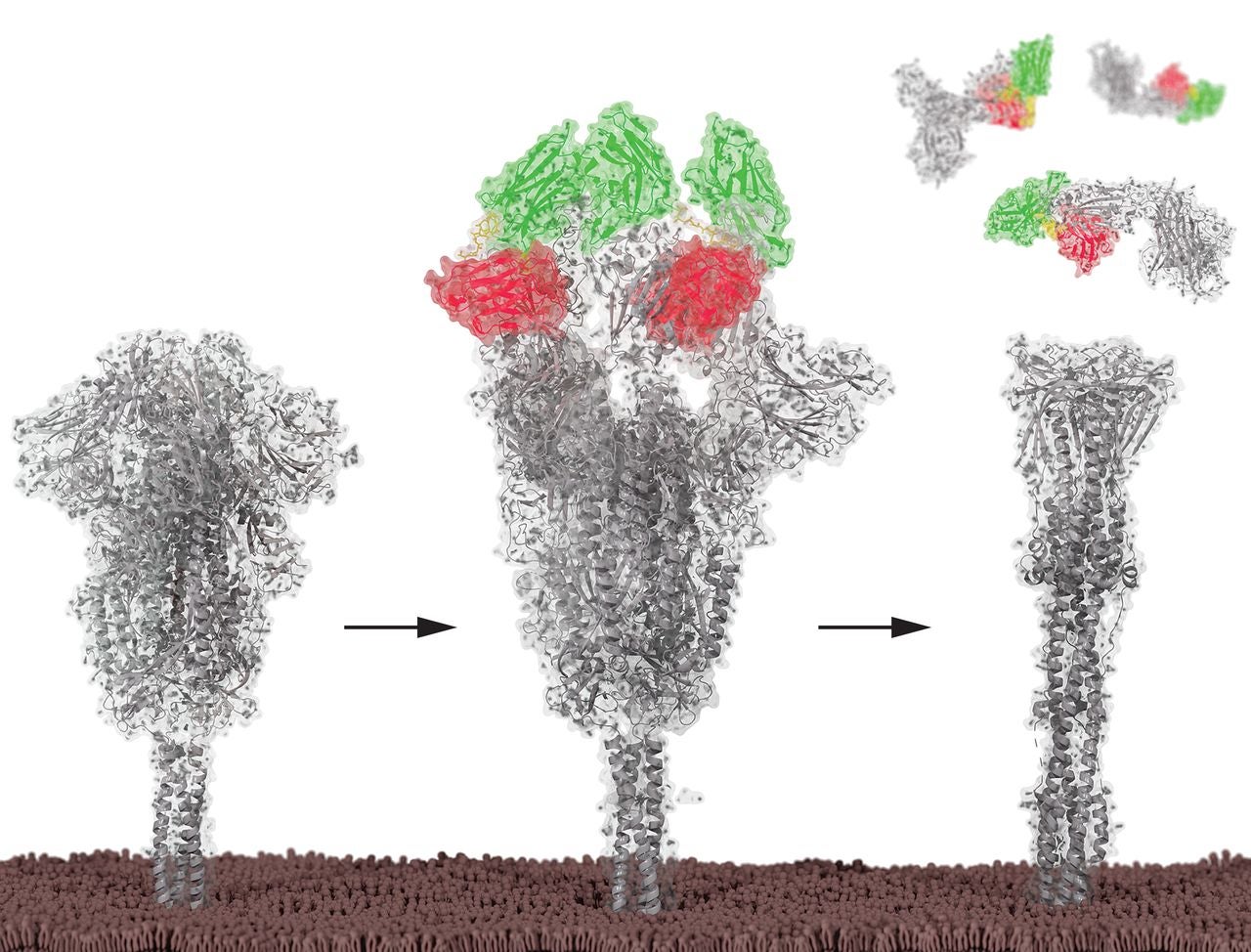 The SARS-CoV-2 spike protein, shown in gray, can be inactivated by nanobodies, shown in red and green. When the nanobodies stick to the spike protein, they cause it to adopt a shape that prevents it from being able to infect cells, researchers recently reported in Science. CREDIT: P.A. KOENIG ET AL / SCIENCE 2021
The SARS-CoV-2 spike protein, shown in gray, can be inactivated by nanobodies, shown in red and green. When the nanobodies stick to the spike protein, they cause it to adopt a shape that prevents it from being able to infect cells, researchers recently reported in Science. CREDIT: P.A. KOENIG ET AL / SCIENCE 2021
Mini antibodies might be delivered via mRNA technology so the antibodies assemble inside people’s cells, Tham says. Vaccine-like injections might work against other infectious diseases, counter toxins such as botulism, or even deliver therapeutics for cancer or other conditions.
And with a simple pill, mini antibodies could be delivered directly to the gut, which could help to block a number of pathogens, for example rotavirus, that enter the body through the digestive tract. Small microbes — such as yeast, bacteria and algae — can’t efficiently make full-size antibodies because these are too complex. However, researchers have proposed genetically engineering spirulina (a blue-green alga that’s often sold as a nutritional supplement) or harmless bacteria called Lactobacilli or Lactococcus that could deliver therapeutic nanobodies via a pill, which would be much more cost effective than producing a drug, Tham says.
Sleuthing cell mysteries
The diminutive antibodies are also a boon for scientists who study proteins and investigate interactions between molecules. The size and long finger of these antibodies can help solve protein structures, map proteins inside cells and show how molecules within cells interact with each other.
Researchers recently solved the structure of a human protein called ASIC1a, for example — it forms a type of channel that lets sodium into nerve cells and plays an important role in pain perception and several neurodegenerative diseases. Stabilizing the protein with a nanobody allowed the researchers to determine its structure with greater resolution, the team reported in 2021 in eLife.
Single-domain antibodies “have the potential of mapping interactions that would be very difficult to study otherwise,” says Ploegh, coauthor of an overview of their traits in the 2018 Annual Review of Immunology. Scientists are even investigating their potential use in the brain — a tricky task because the blood-brain barrier likes to keep foreign molecules out. An international team recently reported using nanobodies as sensors to study whether or not a protein in a mouse brain was activated, and where it was located.
Ploegh says that mini antibodies are exceptionally useful and have significant advantages over full-size antibodies, but they remain somewhat niche because of limited access to the animals that make them — not every researcher has nearby camels, llamas or, in LeBeau’s case, sharks. (“Probably very few people are crazy enough to actually build a shark tank and work with sharks. But we are,” LeBeau says.)
But this is starting to change as interest ramps up. Researchers are also developing new approaches, such as creating synthetic nanobodies and developing mice with “camelized” immune systems for research.
Scientists still don’t know why camelids and cartilaginous fishes, like sharks, are the only animals known to make heavy chain antibodies. Sharks are the most ancient living organisms to rely on antibodies as part of their immune systems, and their antibodies are more stable than those of camelids. Scientists speculate that sharks rely on these antibodies because of the high concentrations of urea in their blood, which would degrade the antibodies of most mammals.
Sharks evolved some 350 million years before camels, yet camelid heavy chain antibodies are also relatively ancient: They are found in both Old World camelids, like camels, and New World camelids, like llamas and alpacas, suggesting that the antibodies may have developed early in the lineage’s evolution. Perhaps “there are certain pathogens that are unique to the camelids that are best fought with these heavy chain antibodies,” Ploegh says.
The heavy chain antibodies of sharks might well be the most ancient immune molecules still in existence — but LeBeau is exuberant about what they could accomplish in the future. “Whenever you work with them, you see something new every day. And that’s really exciting,” he says.
And as for his two-foot-long sharks, when they outgrow their tank, they’ll retire to the local aquarium.
10.1146/knowable-021623-1
Christina Szalinski is a freelance science writer based near Philadelphia. She earned a PhD in cell biology from the University of Pittsburgh. Find her on Twitter: @ChristinaSzal.
This article originally appeared in Knowable Magazine, an independent journalistic endeavor from Annual Reviews. Sign up for the newsletter.